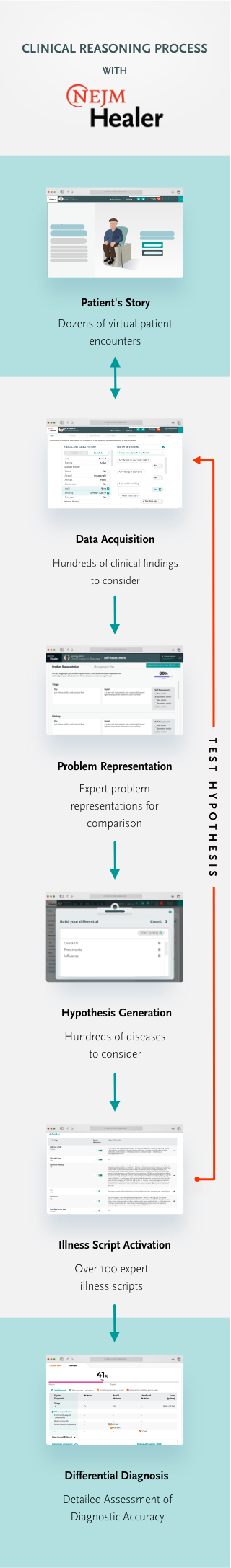
Clinical reasoning is a multi-step, iterative process, often opaque and difficult to convey.
NEJM Healer offers a new way to explicitly teach and assess these cognitive steps. It makes clinical reasoning easier for educators to teach and for learners to master, helping to improve patient diagnosis, management, and outcomes.
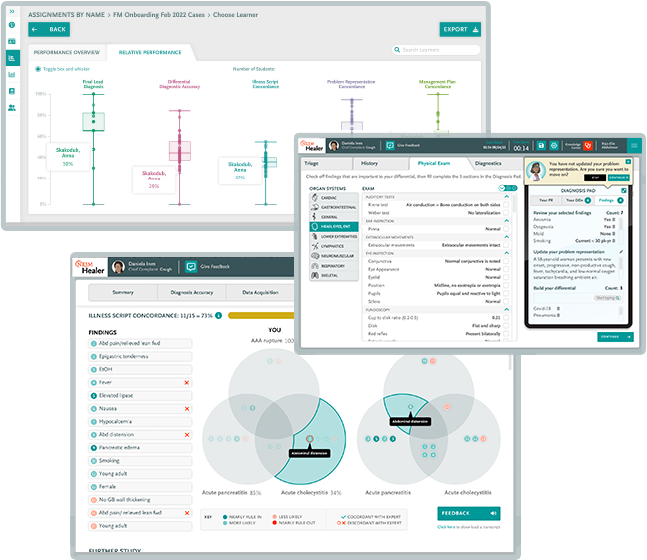
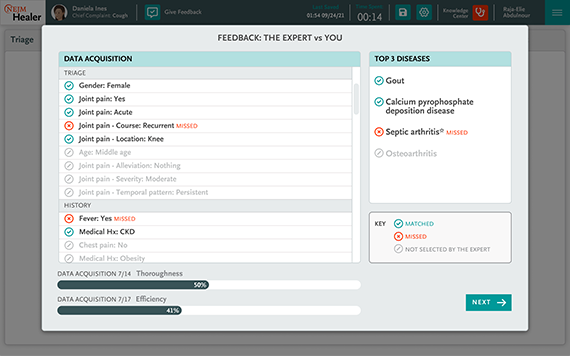
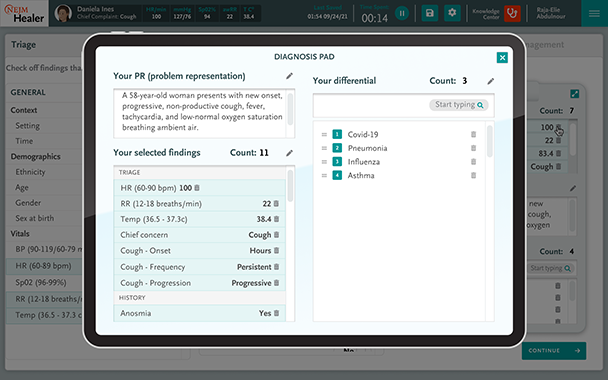
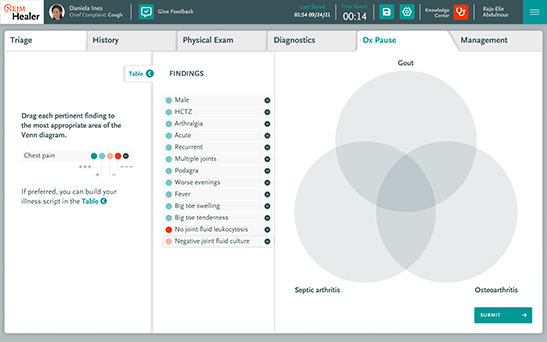
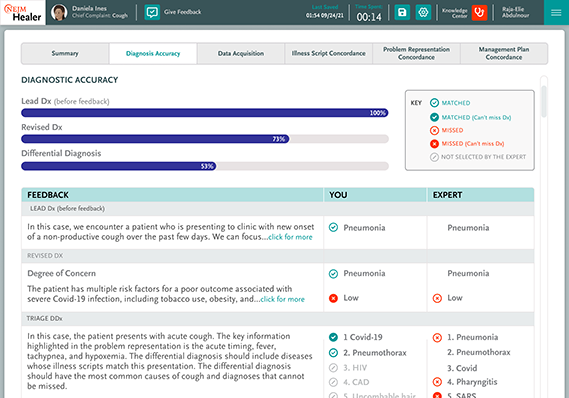
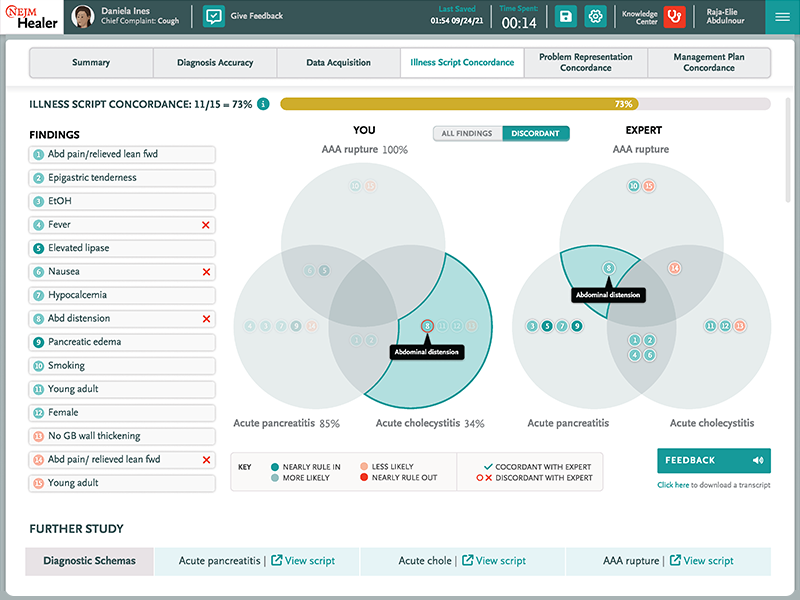
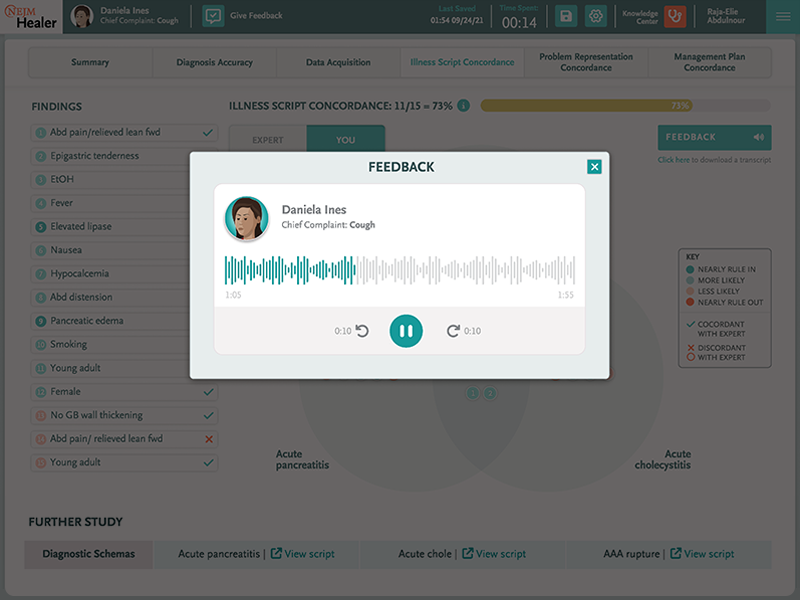
NEJM Healer demystifies clinical reasoning for learners and educators alike by breaking down the key elements of this complex process into discrete, but related skills of data acquisition, problem representation, hypothesis generation, and differential diagnosis. NEJM Healer offers a granular approach to practicing these skills while journeying through the stages of a clinical encounter, allowing learners to understand the reasoning process at a deep level while also yielding detailed and meaningful feedback for the learner and assessment insights for educators.
Through deliberate practice involving many clinical scenarios and disease processes, learners can use NEJM Healer to increase their self-awareness and their confidence, build and refine their clinical knowledge, and learn to apply sound clinical reasoning to any patient case they may encounter.