NEJM Healer offers a systematic way to develop clinical reasoning skills through deliberate practice.
NEJM Healer packages the most current and reliable clinical information in an expansive library of patient cases with a data-driven approach to clinical encounters.
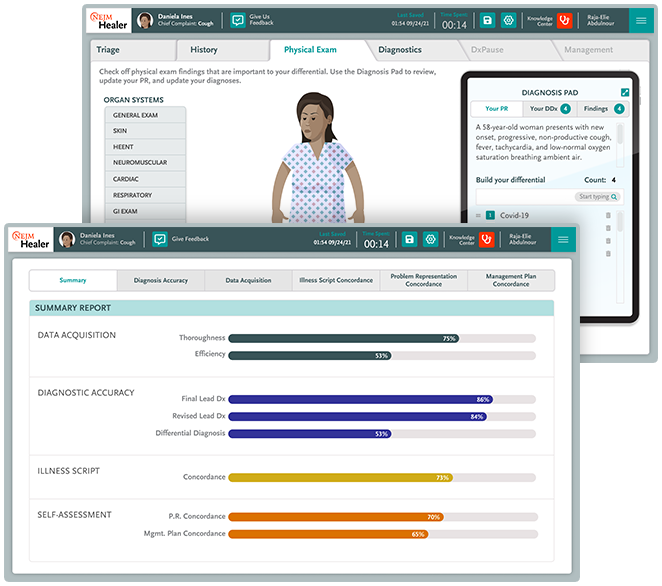
Using NEJM Healer, physician assistant (PA) students engage in realistic virtual patient encounters that range from simple to complex. They learn how to gather and evaluate data, create iterative problem representations, activate illness scripts, build broad differential diagnoses, and apply clinical knowledge to home in on a lead diagnosis. They also create a sound management plan based on the lead diagnosis.
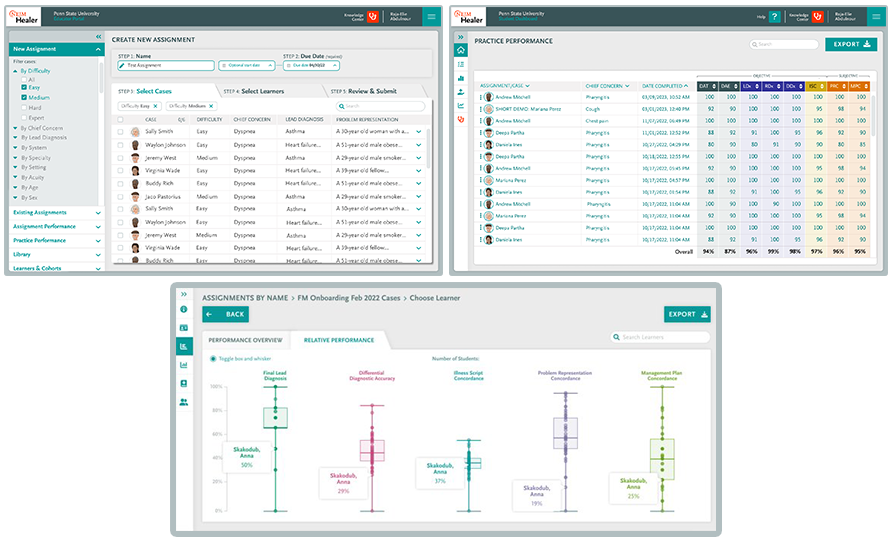
Educators can monitor a student’s path to sound clinical reasoning and diagnosis through a virtual fingerprint of each student’s data-gathering and decision-making history, helping them to identify students in need of remediation and determine which students are ready to move along in their curriculum.